 This blog post is based via interaction on the AskDrBurt a Question Blog. This is a real case, real patient who is searching for a solution to his never ending pain. It is a very long post and if you are a health care practitioner feel free to add your professional advice in a comment area. If you are a reader, and also have health related problems without a solution from your current medical practitioner please contact me via AskDrBurt a Question?
This blog post is based via interaction on the AskDrBurt a Question Blog. This is a real case, real patient who is searching for a solution to his never ending pain. It is a very long post and if you are a health care practitioner feel free to add your professional advice in a comment area. If you are a reader, and also have health related problems without a solution from your current medical practitioner please contact me via AskDrBurt a Question?
Thanks for the very concise and informative blogs Dr. Burt! I would like to ask for advice on presenting my symptoms to health care providers. I have been suffering TMJ symptoms for at least two decades if not more, but none of my health care providers wanted to consider TMJ disorder as a cause. Instead they seem to dismiss the idea and only treat symptoms when they’ve become severe and pretty blatantly obvious. Background/History:
1. Had a fall at age 10 (I’ll be 40 this year) that fractured/dislocated my jaw. No treatment at the time, as it appeared the injury would self heal and any manipulation might affect growth. Since that fall my jaw has always locked, popped,and grinded. It is also very small and my lower teeth have always been crowded.
2. Had ‘braces’ from age 12-14, doc seemed to push my lower jaw back when fitting a bite position for me, and it was always uncomfortable. My lower teeth are extremely crowded and within 2 months after removal of braces/retainer several of the teeth moved back again due to crowding, affecting any hope of a normal bite.
3. Have had significant tinnitus and frequent unexplained ear aches and jaw pains for years. Was told in early 2000’s that I grind my teeth very loudly at night.
4. In 2005 I cracked a 2nd to back/upper molar by night grinding. Began wearing a ‘boil and bite’ mouth guard’ (haven’t had dental insurance, didn’t prioritize or couldn’t afford a custom guard).
5. In 2006, I cracked a lower 2nd/back molar, and had to have it crowned. Still wearing a mouth guard, I cracked both the temp crown and the permanent crown through night grinding.
6. Bought a tempurpedic matress topper and tempurpedic cervical pillow in hopes the highly recommended product/brand would alleviate some of the grinding. It has helped and improved sleep quality too!
6. After that experience, I gave up caffeine, stopped any gum chewing (never was much for it anyhow), began eating organics, regular yoga and massage, and between 06 and present consulted with a family therapist for work stresses as needed. I do regular cervical stretches (provided by physical therapist) get massages and do TMJ self-massages. Life is very low stress right now (got my masters in 2010 and it’s my only debt, woohoo!) but my symptoms continue to worsen, which is pretty stressful as now I’m in constant pain. I am very fit and active, but very gentle on my neck/head with any activities. Unfortunately I’ve had to eliminate all but gentle stretching over the last 6 months due to neck/jaw/upper trap muscle spasms.
7. In 2008, after suffering pain, burning and numbness in my face, neck, shoulder, arms and hands, with loss of fine motor skills in my hands/fingers, I was diagnosed with a completely dessicated C-6/7 and a nerve-compressing herniation at 5/6. Orthopod performed dual discectomy and fusion with plate and screws. He informed me my pain tolerance was very high and I should be cautious of anything ‘uncomfortable’ vs. letting things become painful before seeking medical care. He tried Flexeril (and then Amrix), Mobic, and Vicodin as needed for 3 months before surgery. I asked if I would participate in physical therapy after surgery, but he said no the surgery should fix everything. There was no trauma, no accident, no specific injury that lead to this situation. Doc even diagnosed ‘undetermined’ for the cause. Seems a bit unusual to do that much damage and not want to find or diagnose a cause?!?
8. About 6 months later I began noticing the return of the hypertonacity in my SCM, levators,UT, and rhomboids. Last summer I gave up working out all together (other than stretches), my doctor put me on flexeril, which did very little for 6 months. In December she sent me to physical therapy (severe loss of range of motion in side to side neck movements, and severe loss of motor functioning in my hands with new burning/numbness). PT performed chiropractic manipulations from the thoracic region up to my c-spine, a minimal (maybe 2-3 minutes max) amount of muscle manipulation (the area directly to either side of my spine, thoracic up to c-spine), and traction 3x a week for 6 weeks. He also gave me some shoulder stabilizing exercises which did provide great and quick relief to a quickly rounding posture. I continue those at home. The PT provided temporary relief of the symptoms in my hands/arms but the neck/jaw/upper back symptoms remained, and any week that I was not able to get
all 3 sessions (Christmas and New Years the office closed), my symptoms came back within 3-4 days. 2 weeks after the end of PT, I was back to my original limitations and pain.
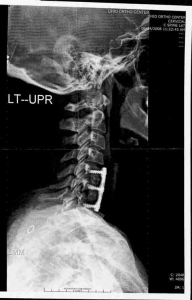
Last week my primary sent me for X-ray (TMJ specific) and a new C-spine MRI. She also ordered a TMJ specific MRI but that has not yet been scheduled. Waiting for the doc to call for my follow up post radiologist report. A good friend of mine is a radiologist in CA, so I sent him a copy of my films, and anecdotally (as a friend and I realize it’s not considered the best practice) he noted what appears to be a significant herniation at C-3/4 on the MRI. The x-rays were not of very good quality and he suggested I may need new films, but he said it was clear that my disc is no longer recognizable in the TMJ joints, there is significant condyle (sp) degredation and evidence of adhesions.
In addition, I have been treated at the same dentist office by 2 dentists since 2008 and have always asked about my jaw issues, and noted that the only way the dentist could even work on my back teeth was for me to manually dislocate my jaw to open it wide enough. My dentist has been replacing amalgam fillings with composite to ensure better strength of those teeth that formed cavities in my childhood (havent’ had a cavity since 1982). At one point, my original dentist stated she wanted me to see a maxillo facial surgeon before completing my work, the last of which was to replace the crown I destroyed in 06 (yes, I dealt with the searing sensitivity of a ‘nub’ for 5 years..I can tolerate a significant amount of pain, and I have always been VERY particular with my dental care). She left the practice before finishing the work, and my new dentist avoided the subject on several occasions when I mentioned the referral. He said ‘we don’t refer unless things are bad’…to which I let him know my history of symptoms, self treatment, and injury from ‘unknown cause’. His reaction ‘yeah, wow that IS kind of bad”. End of discussion. He encouraged me to have the last crown placed, despite my voicing concerns that it would increase TMJ grinding, but he said it wouldn’t be a problem if he gave the crown a low profile. He was absolutely wrong. I have had to go back for 2 sessions of dental work where the crown surface was lowered, and the two teeth surrounding the crown, and one on the top jaw have also needed reduced as they are not under greater pressure with the new crown placement.
The only consistency in 30 years has been the night bruxism. The rest of my spine is happy and healthy, and symptoms have progressively radiated from the TMJ area down my head, neck and arms.
I apologize for the mini-novel, and if you can give any guidance I will be extremely grateful. I’m at the end of my wits as to why practitioners continually ignored that something was at the root of my symptoms as the symptoms have been significant. I now am wondering what can possibly be done if 3/4 is severely herniated as I already have 3 vertabra fused in my C spine?!? I don’t want to become disabled or severely limited, and if that’s the case I’m beyond frustrated that none of my practitioners ‘stepped up’ to give this proper attention. Any suggestion made by a practitioner has been followed to a T, but those have been rare. As of late, I started seeing a new primary and she is very interested in helping me come to the root of my symptoms, thank goodness.
I feel I am articulate (sorry, I know verbose fits this note as well) intelligent, patient, motivated, very healthy, active, self-aware, avoid any and all medications unless necessary, and find preventative care (such as healthful living, stress reduction, massage, chiropractic, etc) to be the best way to lead a healthy life.
So, how can I share this succinctly with practitioners as we go forward in the process of discovering a cause and hopefully finding solutions for the cause vs. remedying damaging and continual symptoms? I don’t want to sound whiny or self-involved, but after 30 years of this, and at least 10 years of being handed off to someone else or some other practitioner….only to utilize their every resource and still have issues (hello, TMJ disorder anyone?) I’ve lived through more pain, limitation and frustration than a person should expect in this day and age with our advanced medical system.
Thank you so very much for your time. I appreciate any advice. Confidentiality and discretion is also appreciated 
Dr. Burt’s Answer:
Got your message via AskDrBurt a question. Long history of problems that have been avoided, ignored or misdiagnosed in the past. My main concern is the surgery that was performed on your cervical spine. Post surgical scar tissue formation is the main cause of excessive pain in your cervical spine. No Post Surgical rehabilitation was performed, such s physical therapy. I do not understand how come your surgeon said:”The surgery will fix the problem.” WOW. Limited ROM is making things even worse in your neck. Intervertebral discs stop getting their nutrition the moment the two adjacent vertebraes stop moving – process called imbibition. Solution – life long manual cervical distraction and maintaining whatever is left of a cervical lordosis. I have couple of products on my blog that would be of a great benefit to you. If you are interested I could send you direct links and you can evaluate them.
TMJ – TMJ is very closely related to a cervical spine. There is a close neurological relationship between TMJ and Cervical Vertebral Joints. The question is – did your jaw healed properly after it was fractured? If yes, then there is still some hope in correcting by special cranial work (S.O.T. technique – Sacro Occipital Technique) It is very hard for me to provide more recommendations as I would actually need to see, examine, evaluate and make my own diagnosis with areas of concern. Doctors of Chiropractic look at the health related problems from the causation point of view and not symptoms point of view. Find the cause and the problem will be fixed. Feel free to ask any additional questions. Perhaps by helping to find the proper solution to your problem is going to be the first step, second would be to find the proper health care practitioners.
PS: Would you like me to post your health history and the problems that you had with previous doctors on my blog? can keep your name confidential if you like, so no one will know who you are. This will open a door to many other health care providers reading your story and possibly commenting and adding valuable advice to your health related problem.
Talk to you later
Reader’s Response:
Wow, thank you so much for your prompt response! I couldn’t agree more with your statement that fixing the cause usually resolves the symptoms, and that is my main mission now.
Unfortunately, the jaw was never re-evaluated after the initial fracture/dislocation at age 10. If I had to estimate, I would say ‘no’ as that’s precisely when the popping, locking, grinding sounds upon movement began.
Considering I only have the axis, atlas, 3 and 4 discs left in my c-spine (not sure I got the anatomy properly identified with those terms) I have always done as much to keep range of motion functional post surgery. 2×3 times a day I use a heat pack (dry rice wrapped in flannel) stretching under warm shower, and PT generated cervical stretches (I also use a stretching strap, theracane, pro-stretch for calves and mini-tough tennis ball to roll the balls of my feet, and a foam roller for myofascia release), and now spend most of my time at a standing desk, as only standing and flat supine laying down do not cause significant pain/numbness….if it can help, and it’s not surgical or drugs, I’m willing to try it. Please do send me links to the products you mentioned and I will determine if they are within my budget. Unfortunately I’ve not been able to work much due to the pain and the limited amount of time I can spend seated during travel, ugh!
Another concern….should I be wary of the x-rays recently taken…as the tech had me lie in a prone position and placed my head on what was like a slightly inclined podium on the x-ray table? How could joint position possibly be properly evaluated since I have a hard time with ROM on rotation, and the pressure point ended up right ON the TMJ area? Tech had to take 5 attempts on the left side, 8 on the right. In addition the MRI tech decided against the deliberately ordered contrast for the MRI, and there appears to be a black blurred area around my fusion and above due to the titanium. I would certainly have traveled to a larger metropolitan area if I had the funds available, but as an entrepreneur I’m without health insurance at present. I KNOW things will get better, I KNOW this will pass.
I suppose it can’t be too terribly invasive to post my information after removing identity…please feel free to edit anything as you see fit if it will make it more relevant to other practitioners.
I understand you cannot evaluate beyond the anecdotal information but I cannot tell you how absolutely grateful I am for your consideration and suggestions.
Again, thank you from the bottom of my heart for your reply, suggestions and care. If there is anything I can do to promote your business, your blog (through my blog) or your products please do not hesitate to share that process with me. I will oblige and remain extremely grateful.
Attached the x-ray taken a few weeks after the fusion 09 June 2008. What lordosis, ha!?! Sorry that IS humor albeit sarcasm…if we can’t laugh at ourselves…… ;0)
Very Gratefully,
Reader wished to keep his identity anonymous.
Dr. Burt’s Answer:
Hello again,
I agree with you 100% that your X-Ray tech just radiated you for nothing. Spine is a weight bearing structure and responds to weight bearing stresses. You could see better what is going with the spine when you shoot X-Rays in a standing position. Full spine X-Ray is an optimal if possible. Lower back problems are related to your neck problems. Every single subluxation and curve in a cervical, thoracic and lumbar spine must be taken into consideration in order to achieve the best results possible. I would not expose myself a second time to an additional dose of radiation at this point and time. The is still a small presence of cervical lordosis which is a positive sign. There is nothing that can be done at this point and time with your lower cervical spine. Sorry to say, but too much damage has been done by your orthopedic surgeon. The goal at this point is to keep the vertebraes and IVD (Intervertebral discs) from degenerating farther. If I would be you I would get these two products: #1. Bodyline BDL127 The Neck Decompressor and #2 Posture Pro Corp. POS107 Deluxe Full Spine Posture Pump Model 4100
Neck Decompressor will keep your IVD healthy and Posture Pump will help to keep cervical and lumbar lordosis in order. I use these products on myself and the members of family.
When the blog post will go live you can continue the conversation via DISQUS, thus many other doctors can add value to your condition.



















